As an anesthesiologist and clinical leader, I have your typical mix of responsibilities, including clinical loan, scheduling, and hospital committee work. I am also the lead recruiter of our group, which has given me a firsthand look at how physicians approach their first job offers—and how awkward and uncomfortable salary discussions can be in medicine.
I still recall a negotiating experience from a few years ago with an anesthesiology resident. Unlike most others who are excited to land their first big paycheck job out of residency, he came in fully prepared to negotiate. He first tried negotiating his base and bonus, but an adjustment like that would mean changing comp across our entire group. So, he moved on to his signing bonus and then to relocation expenses. He tried to negotiate his package wherever possible, and ultimately, he got much more than what was customary. I was genuinely impressed by how well he advocated for himself.
That incident has stuck with me—not because of how persistent he was but because of how prepared he was. He had data. He knew what to ask for. He had worked hard to get all the information, and it reminded me how little salary transparency there is in medicine and what’s possible when you have the information and the confidence to advocate for yourself.
This is why I started Marit—a community-powered anonymous salary-sharing site built for medicine. Using real, anonymized salary submissions from thousands of physicians around the country, we've compiled detailed compensation data for all of medicine, where you can see all the averages and, more importantly, the details that matter—from comp model to bonuses to schedule and shifts, benefits, etc.
Most salary benchmarks typically publish averages across all career levels—whether you are fresh out of residency or 15 years into your attending career. That’s not particularly helpful for new grads, so in this post, we'll present a unique view of data, specifically filtered for new attendings (i.e., those with less than two years of experience). If you’re preparing to negotiate your first offer, this should give you a clearer sense of what might be possible.
Core Components of an Offer
When reviewing a new attending offer, it’s easy to focus on the base salary—but that’s only one part of the picture. Most offers include a guaranteed base, but multiple bonuses are often layered on top, tied to things like productivity, quality metrics, etc. Depending on the role, you may also have additional income opportunities, such as overtime or extra shifts.
In the benchmarks below, we’ll focus on total compensation, including all of these components. In addition, there will be one-time payments like sign-on bonuses, relocation support, residency stipends, student loan assistance, and a range of benefits that can vary widely.
More information here:
28 Things You Can Negotiate Besides Salary
12 Negotiation Techniques You Need to Know
How Much Do New Grads Make for Each Specialty?
Here are the average starting salaries for new attending physicians across all specialties, based on the physician salary data on Marit. In addition to salary, we’ve included typical weekly hours worked and a pay satisfaction score. This score is based on a 5-point scale, with 1 representing Very Dissatisfied with Compensation and 5 representing Very Satisfied with Compensation. The average across all specialties is 3.6 stars.
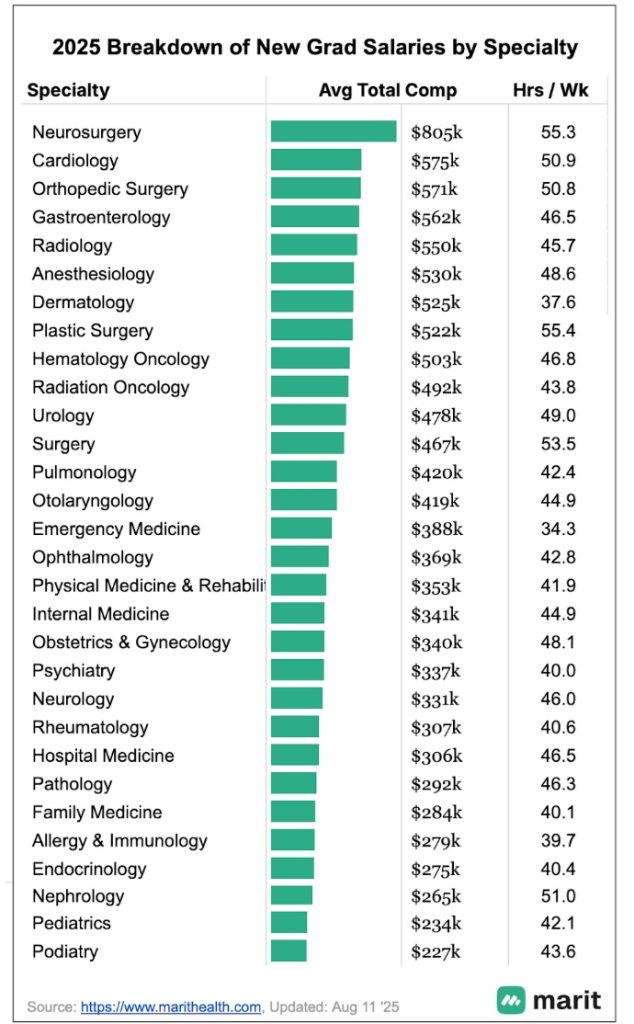
Why the Highest Paying Specialties Stand Out
At the top of the list are neurosurgery ($805,000), cardiology ($575,000), and orthopedic surgery ($571,000). These specialties continue to be consistently among the highest-paying specialties, owing to their heavy procedural volumes and higher reimbursement rates associated with them. On the other end, podiatry ($227,000), pediatrics ($234,000), and nephrology ($265,000) sit at the lower end of the pay scale. These specialties typically generate modest wRVU volumes, and their codes tend to have lower reimbursement rates
More information here:
There Was No Golden Age of Medicine (at Least for Physician Incomes)
‘What Are Your Salary Expectations?’ Here’s Why You Should Stop Evading This Question
Academic vs. Non-Academic Salaries
Keep in mind that these figures represent averages, and there are huge variances depending on factors like practice type, location, compensation structure, and work schedule. One major factor affecting starting salaries is whether you're joining an academic institution or a private hospital/medical group. Here’s how new attending salaries compare between academic and non-academic settings:
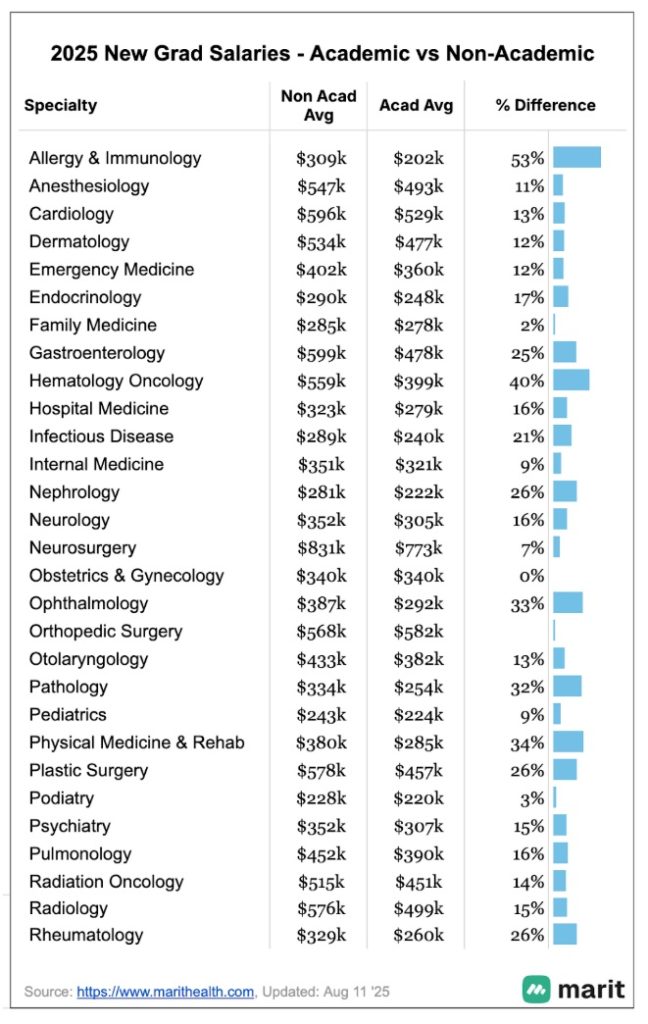
Allergy & immunology shows the largest gap, with non-academic salaries averaging 53% higher. Other specialties with large differences include hematology oncology (40%), physical medicine & rehab (34%), ophthalmology (33%), and pathology (32%). There are many drivers of these differences, but one of the biggest tends to be the amount of clinical workload in each setting. Academic physicians often tend to see fewer patients as they split their team between clinical and non-clinical responsibilities.
Some of the smallest gaps, or no gaps at all, appear in orthopedic surgery, OB/GYN, and family medicine, where academic and non-academic roles both involve heavy clinical loads.
Sign-On Bonuses and Relocation Allowances
Most new attending offers include a sign-on bonus, and this is often one of the more negotiable parts of the package. That said, it’s essential to read the fine print. These bonuses usually come with conditions, such as a requirement to stay with the employer for a certain period (often around three years). If you leave early, you may be required to repay some or all of the bonus.
Based on Marit's dataset, there’s a strong correlation between total compensation and the size of the sign-on bonus. The overall trend is roughly approximated by the following formula:
Sign-on bonus ≈ $5,700 + 7.1% of total compensation.
For example, a new attending earning $400,000 in total comp might expect a signing bonus of roughly $34,100 ($5,700 + 0.071 * $400,000). Keep in mind that actual signing bonuses vary by specialty, employer type, and region, and they tend to be higher for harder-to-fill positions. Still, this can be a helpful benchmark when reviewing or negotiating your offer.
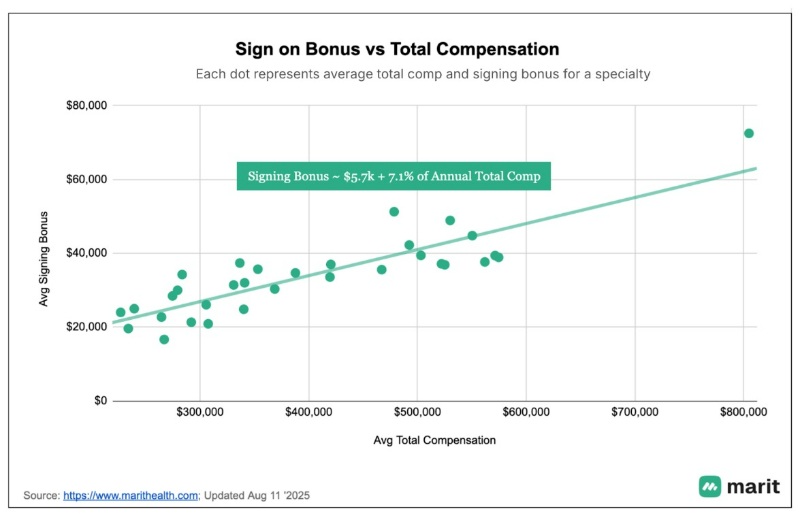
Relocation allowances are more standardized, and they do not vary by specialty as much. The average relocation bonus on Marit is ~$13,000.
More information here:
The Best and Worst Metro Areas for Physician Salaries
Future Growth Prospects
Let’s talk about what happens after that first contract. For most physicians, compensation increases steadily in the early years of practice. Beyond that, salary growth will depend heavily on the choices you make: how much you work, the type of schedule you prefer, your productivity, and the kind of practice you join.
But growth isn’t the same across the board. Some specialties see faster increases than others, driven by factors like how your productivity increases with experience, demand within the specialty, shifts in reimbursement, and broader changes in the healthcare landscape. Below is the specialty-specific growth in compensation we see on Marit, so you can get a better sense of what your earning trajectory might look like over time.
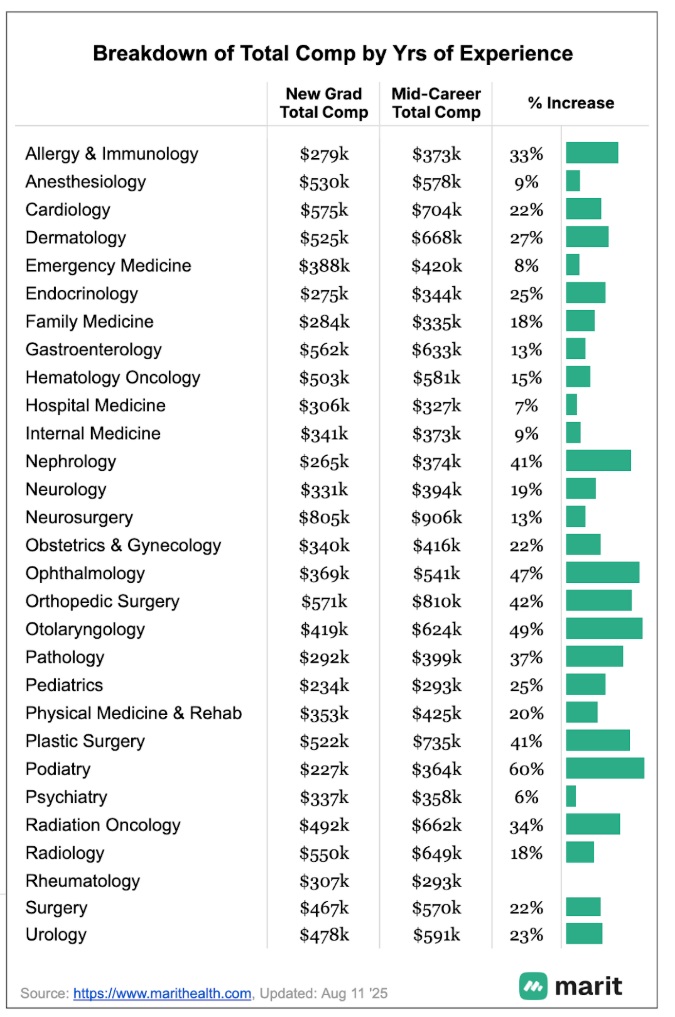
Specialties that have a significant mix of private practice models or rely heavily on productivity-based models—like ENT (+49%), ophthalmology (+47%), orthopedic surgery (+42%), podiatry (+60%)—tend to show the most significant percentage increases. These physicians often start in salaried roles at a larger health system and may transition into a private practice or a productivity-based model, where earnings are more directly tied to volume, collections, or shared group profits. Compensation tends to accelerate as they ramp up productivity or gain access to equity or partnership tracks.
By contrast, specialties with more salary-based structures—such as hospital medicine, emergency medicine, and anesthesiology—have flatter growth curves (all under 10%). These roles often have standardized pay across years of experience, especially in hospital-employed settings, leaving less room for significant increases over time.
We hope this overview was helpful. While salary averages can offer useful benchmarks, every contract is different and shaped by various factors. You can explore the full dataset on Marit for a more detailed view, including real, anonymized salary data broken down by compensation models, locations, hours, benefits, and more.
These deep dives are only possible because of the physicians who have already shared their data. If you found this post valuable, consider submitting your salary anonymously and sharing Marit with a colleague who might benefit.
What's the most important aspect of a new attending's contract: base salary, bonuses, or other kinds of benefits? How much negotiating have you done in your own salary discussions? Are you satisfied with how much you made or currently make as an early-career doctor?
